Assessment and Diagnosis of Fluency Disorder: Individuals are referred to a speech-language pathologist (SLP) for a comprehensive assessment when disfluencies are noted and when one or more of the factors listed below are observed along with the disfluencies. A comprehensive fluency assessment typically includes the following:
Preassessment
- Clinical Questions: It help in determining the developmental/treatment level of the client’s disfluency. For example clinician asking the some question to gathering information about client’s disfluency, What are the amounts and types of disfluency shows in various situations? What kinds of risk factors for stuttering does the client have? Is the client reacting to his speech with frustration, fear, or other emotions?. Clinical questions also help in making referral to another professionals.
- Public School Considerations (in school-age child): The Individuals with Disabilities Education Act (IDEA ’97 and changes made in 2004) and individual state laws mandate the procedures that public school clinicians must use for gathering information about a child’s disability and deciding on treatment. Speech-language pathologists are usually members of a team that consults with the teacher and parents to determine if a child’s difficulty can be resolved by making changes in the educational setting.
- Initial Contact (in preschool child or school-age child): In your initial contact, the family member who has approached you is forming his or her first impression of you.
- Attitude Questionnaires (in adolescents and adults): Assess client’s communication attitudes through observations, interview questions, and questionnaires.
- Case History Form: It informs the clinician about the parents’ current perception of the problem, as well as its onset and development, and the child’s medical, family, and school history.
- Audio/Video Recording: Ask the parents of a preschool child or school age child to send me an audio recording or preferably a video recording of their child speaking in a typical home situation.
Assessment
- Parent-Child Interaction (in preschool child): Gives a more natural sample; gives an opportunity to see the child’s stuttering firsthand; Observe how the parents interact with their child.
- Parent Interview (in preschool or school age child): Gives me a chance to suggest how, in my experience, openness about stuttering decreases some of the shame a child (and parents) may feel about stuttering.
- Interview (in adolescents and adults): Interview with an open-ended question such as, “Tell me the problem that brings you here today,” or “Why don’t you tell me about your stuttering?”
- Teacher Interview (in school-age child): The following questions serve as guidelines for the types of things clinician want to find out – Does the child talk in class? Does he stutter? What is his stuttering like? How does he seem to feel about his stuttering and about himself as a communicator? Does stuttering interfere with the child’s performance in school? Do other children tease him about stuttering? How does the teacher feel about stuttering, and how does he or she react to it?
- Classroom Observation (in school-age child): Direct classroom observation can help clinicians understand the severity of a child’s stuttering and the degree to which it interferes with his academic adjustment.
- Child/Student Interview (in school-age child): Clinician arrange for the child to come to the treatment room. Here, I set about to make him feel that my room is an accepting environment where he can have fun and also discover how he can make his speech much easier.
- Clinician-Child Interaction (in preschool child): the clinician can see firsthand what the child’s speech is like, how he responds to various cues, and how well he can modify his disfluency.
- Talking about Stuttering
- A Child Who Won’t Talk
- A Child Who Is Entirely Fluent
- Speech Sample: The following sections describe how to analyze samples of a preschool child’s speech. You should have more than one speech sample to analyze from the recordings that the parents sent in, the parent-child interaction, and the clinician-child interaction.
- Preliminaries (in school-age child): Record a video with him talking for 10 minutes about school and other activities in the therapy room. record a sample that optimally includes 300 to 400 syllables of his/her speech.
- Pattern of Disfluencies: Frequency of disfluencies; Types of disfluencies; Nature of repetitions and prolongations; Starting and sustaining airflow and phonation; Physical concomitants; Word avoidance.
- Stuttering Severity Instrument (SSI-4): Using the 200-syllable or longer samples gathered earlier, you should carefully follow the guidelines in the examiner’s manual of the SSI-4 to determine a child’s stuttering frequency, duration, and physical concomitants scores.
- Test of Childhood Fluency (in preschool child): Test of Childhood Stuttering (TOCS) can be used for children ages 4 to 12 and is thus appropriate for older preschool children.
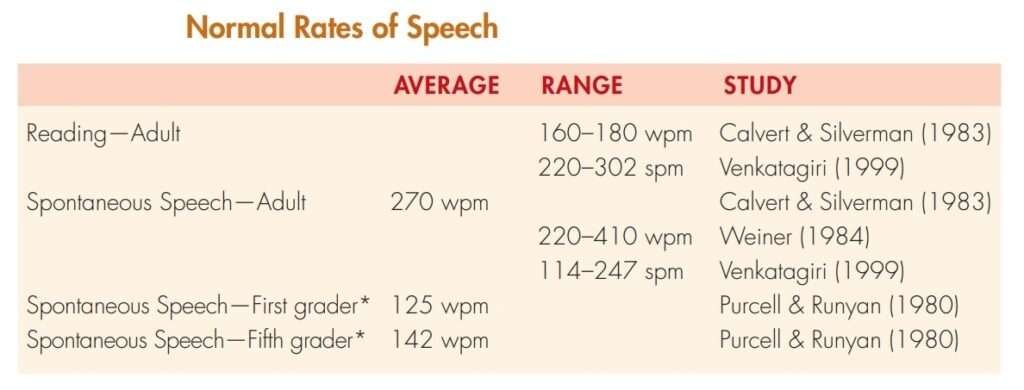
- Speech Rate: Assess preschool children’s speech rate using the speech sample obtained for the SSI-4.

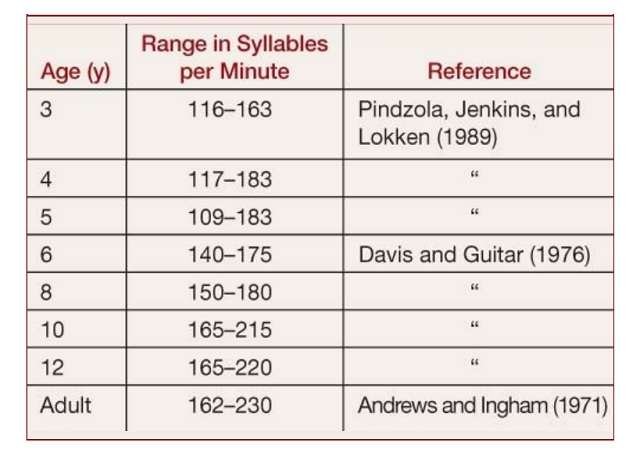
- Other measures of Fluency (in adolescents and adults): Clinician may use audio recorded sample for assessing combination of frequency of stuttering (percentage of syllables stuttered) and speech rate (syllables spoken per minute). These measures,
which were first described in Andrews and Ingham (1971), together require much less time than the SSI.
- Other measures of Fluency (in adolescents and adults): Clinician may use audio recorded sample for assessing combination of frequency of stuttering (percentage of syllables stuttered) and speech rate (syllables spoken per minute). These measures,
- Trail Therapy (in school-age child or adolescents and adults): Trial therapy with a school-age child or adolescents and adults will help me understand what approach might work with this particular client as well as what may be difficult for him. If the client is able to make significant, though temporary changes in his stuttering in this brief treatment, he will gain hope and motivation for our work together.
- Feelings and Attitudes: Asking the parents if they think the child is aware of his stuttering, and I explore observations they have made of his reactions to his disfluencies.
- Other Speech and Language Behaviors: Screen for possible articulation, language, and voice problems. Make sure that his hearing has been checked.
- Other Factors
- Physical Development (in preschool child or school-age child): Child has age appropriate gross motor skills and whether his oral motor development is typical and evolution of his stuttering was associated with his delayed motor development.
- Cognitive Development: There is cognitive delay, which can be associated with increased disfluency.
- Social-Emotional Development: Examine life events surrounding the onset of fluency disorder to see if upsetting events or ongoing situations may be linked to the client’s fluency disorder.
- Speech and Language Environment (in preschool child): Many children have their hands full trying to compete verbally with fast talking, articulate adults. Observe the parent-child interactions carefully for indications of a complicated verbal environment, such as rapid speech models without pauses.
- Academic Adjustment (in school-age child or adolescents and adults): Clinicians can determine if a child needs extra help in certain academic areas through discussions with his teachers about which speaking situations in school are most difficult for him. If the child has more difficulty in certain academic situations, these should be given extra attention in treatment when planning generalization of more fluent speech.
- Intelligence (in adolescents and adults): If a client has below-normal intelligence, he may have difficulty following the regimen of a typical therapy program.
- Psychological adjustment (in adolescents and adults): Psychological problems that are relevant to stuttering also may become apparent during the interview when the onset of stuttering is explored. Sudden onset after a psychological trauma, particularly if onset is in late adolescence or adulthood, may indicate psychogenic stuttering.
- Vocational adjustment (in adolescents and adults): The degree to which an individual succeeds in choosing the kind of work or career best suited to his or her interests, traits, and talents.
Diagnosis
Diagnosis of Preschool age Children
- Determining Developmental and Treatment Level
- Typical Disfluency: 10 or fewer disfluencies per 100 words; mostly of multisyllable word and phrase repetitions, revisions, and interjections.
- Borderline Stuttering: 11 or more disfluencies per 100 words; They may be part-word repetitions and single-syllable word repetitions, as well as prolongations, and the repetitions may have more than two repeated units per instance.
- Beginning Stuttering: rapid, abrupt repetitions; pitch rises during repetitions and prolongations; difficulty starting airflow or phonation; and signs of facial tension.
- Risk Factors for Persistent Stuttering: Constitutional, Developmental, Environmental, and Learning Factors.
Diagnosis of School-age Children
- Most school children are at beginning or intermediate levels of stuttering.
- Beginning-level stuttering is characterized by physical tension, hurry, escape behaviors, awareness of difficulty, and feelings of frustration.
- Intermediate level: Blocks in which sound and airflow are shut off; also involves tension, hurry, escape behaviors, and frustration, as well as avoidance behaviors as a result of fear and anticipation of stuttering.
Diagnosis of Adolescents and Adults
- Intermediate Level: Blocks in which sound and airflow are shut off; also involves tension, hurry, escape behaviors, and frustration, as well as avoidance behaviors as a result of fear and anticipation of stuttering.
- Advance Level: Long, tense blocks; some with tremor; Escape and avoidance behaviors present.
References:
⇒ STUTTERING An Integrated Approach to Its Nature and Treatment – BARRY GUITAR, PH.D. (Book)
⇒ ASSESSMENT in Speech-Language Pathology A Resource Manual -Kenneth G. Shipley Julie G. McAfee (Book)
⇒ Fluency Disorders – ASHA
You are reading about:
Assessment and Diagnosis of Fluency Disorder






0 Comments